Deep Vein Thrombosis (DVT): A Comprehensive Guide
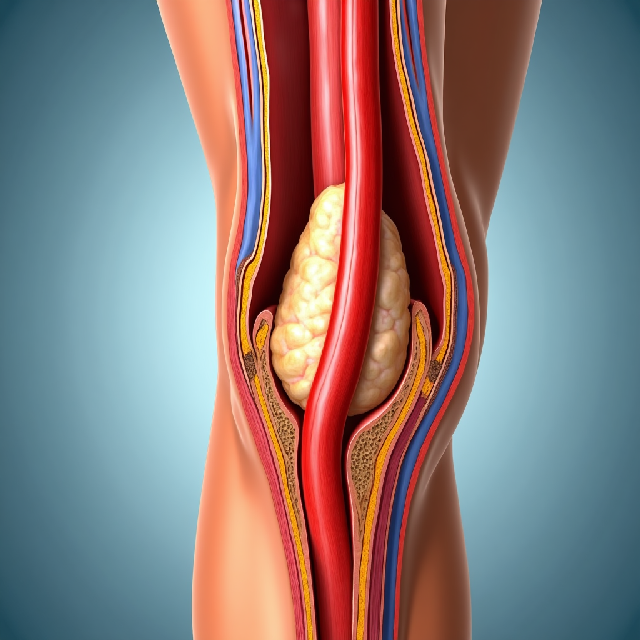
Deep Vein Thrombosis (DVT) is a serious medical condition where blood clots form in the deep veins, typically in the legs. These clots can block blood flow and lead to life-threatening complications if not treated promptly.
Why DVT Matters
- Leading Cause of Pulmonary Embolism: DVT is a major cause of pulmonary embolism (PE), where the clot travels to the lungs, potentially causing death.
- High Mortality Rates: It contributes significantly to cardiovascular-related deaths, ranking third after heart attacks and strokes.
- Long-Term Health Impact: Even if not fatal, DVT can lead to chronic conditions like post-thrombotic syndrome, affecting quality of life.
Understanding Blood Clot Formation
Blood clots are crucial for stopping bleeding but can be dangerous when they form unnecessarily. The process involves:
Coagulation Factors
These proteins activate in a cascade, leading to thrombin formation, which converts fibrinogen into fibrin strands that trap platelets and cells.
Platelet Activation
Platelets stick to damaged areas and release chemicals, forming a temporary plug that signals fibrin clot formation.
Fibrin Polymerization
Thrombin converts fibrinogen into fibrin, creating a mesh-like structure that traps blood components.
Emerging Research
Scientists use computational models to simulate clot formation, aiding in treatment development without human trials. These models help understand clot strength and flexibility.
Recognizing DVT Symptoms
Early detection is crucial for preventing complications. Common symptoms include:
- Pain or Cramping: Persistent pain in the leg, often starting in the calf.
- Swelling: The affected limb may become visibly swollen or tight.
- Redness and Warmth: Skin inflammation caused by the clot.
- Asymptomatic Cases: Up to 70% of cases may not show symptoms, especially in smaller veins.
Risks and Complications
Pulmonary Embolism (PE)
A life-threatening complication where clots block lung blood flow. Symptoms include sudden shortness of breath and chest pain. Early detection with CT pulmonary angiography is crucial.
Post-Thrombotic Syndrome (PTS)
Affects up to 50% of DVT patients, causing chronic swelling, pain, and skin discoloration due to damaged veins.
Risk Factors
- Immobility: Prolonged inactivity increases clot risk.
- Surgery: Major procedures can damage veins.
- Cancer: Increases blood’s tendency to clot.
- Genetics: Conditions like Factor V Leiden heighten DVT risk.
Diagnosis Methods
Accurate and timely diagnosis is essential:
-
Imaging Techniques:
- Duplex Ultrasound: Standard test combining ultrasound with Doppler technology.
- CT Scan: Detects clots in legs and lungs.
- MRI: Useful for detecting pelvic or thigh clots.
-
D-dimer Blood Test Measures a protein fragment from broken clots, though not definitive alone.
-
Clinical Prediction Indices Tools like Wells Score assess risk factors to guide testing.
Treatment Options
Anticoagulant Therapies
- Heparin: Quick-acting, often initial treatment.
- Warfarin: Oral option requiring INR monitoring.
- DOACs: Fixed-dose alternatives without blood tests.
Compression Stockings
Graduated pressure improves blood flow and reduces swelling.
Mechanical Interventions
- Thrombolysis: Dissolves clots in severe cases.
- Surgical Thrombectomy: Removes clots when necessary.
Emerging Research Directions
-
Robotic-Assisted Ultrasound Improves accuracy and extends diagnostic reach to remote areas.
-
Mechanical Thrombectomy Devices Non-surgical clot removal, reducing recovery time.
-
Inflammation and Immune Response Understanding immune mechanisms may lead to targeted therapies.
Conclusion
DVT demands attention due to its potential complications. Early intervention can save lives. If symptoms arise, seek medical help immediately. Share this guide to spread awareness about DVT detection and treatment.
I’m curious about how the article validates computational models for DVT research and their impact on drug development and personalized treatments. I’d also like to know if the approach considers individual factors like genetics, lifestyle, and environment to create more effective therapies.
Thanks for your great points! The article explains how scientists use computer models to study clot formation, helping them learn about strength and flexibility without needing human trials. However, it doesn’t clarify how these models are tested or their role in creating new treatments. Your point about personalized therapies considering genetics, lifestyle, etc., is spot on. It would be great if the article shared whether these models can include such personal factors to improve treatment customization.
The article discusses computational models for clot formation but doesn’t detail their validation or role in treatment development. I wonder if they consider factors like genetics and lifestyle to aid personalized therapies.
The article talks about computational models simulating clot formation to help develop treatments without human trials but doesn’t explain how these models are validated or used in real drug development. Your idea of including personal factors like genetics and lifestyle is smart, as personalized approaches can make therapies more effective. It would be helpful if the article provided more details on whether these models account for such individual differences to improve treatment customization.